Emergent treatment of aortic rupture in acute type B dissection
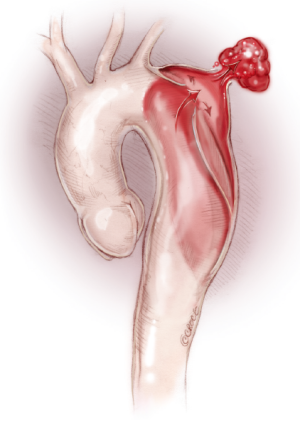
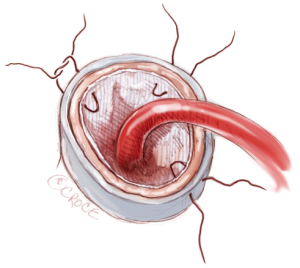
Aortic rupture with massive left hemothorax is a catastrophic complication of acute type B aortic dissection (Figure 1). This is associated with high mortality, due to primarily hemorrhagic shock and hypotension. In this setting, treatment is usually represented by open surgery and/or thoracic endovascular repair (TEVAR). TEVAR is currently the most frequently adopted management; however, its planning in these emergent patients may be very difficult. In emergency, important issues include: (I) presence of a proximal intimal tear in the left hemiarch and absence of useful and safe proximal aortic neck; (II) undersized aortic diameter at preoperative CT scan related to the hypotension; and (III) unavailability of the proper endograft size in that moment.
First stage-TEVAR
Clinical presentation
Hypotension: hemorrhagic shock (mean arterial pressure <50/0 mmHg, Hb <5 g/dL).
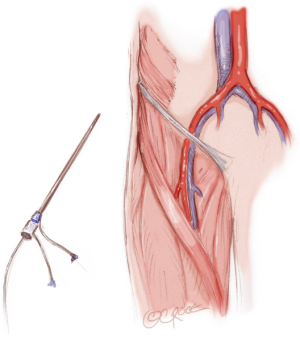
Sizing and preparation
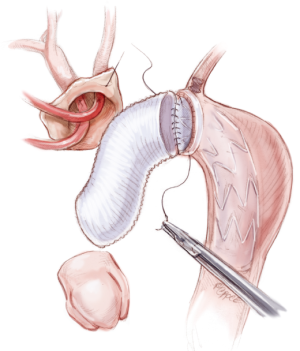
The patient is placed in a supine position. Under general anesthesia, right femoral artery access is achieved, and the appropriate endograft size selected (Figure 2).
Operation
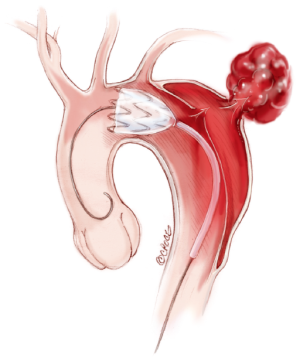
The stent-graft is introduced with a percutaneous or cut-down technique to cover promptly the proximal entry tear and rupture (Figure 3).
The stent-graft is placed in the left hemi-arch, zone 2 based on the Ishimura classification, between the origin of the left common carotid artery and the origin of the left subclavian artery (LSA) (Figure 3).
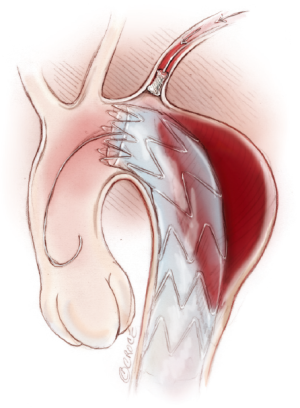
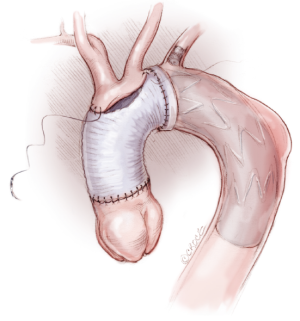
LSA endovascular closure is performed to avoid type II endoleak (Vascular Plug). In emergency there’s no indication to left carotid-subclavian artery bypass (Figure 4).
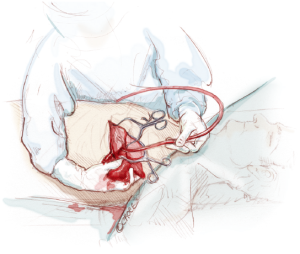
Hemothorax drainage can then be achieved via left thoracotomy (Figure 5).
Postoperative course
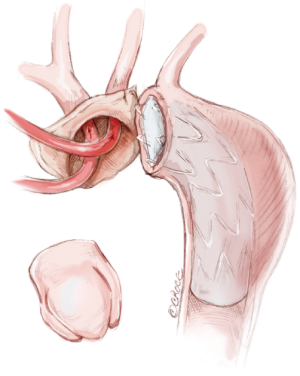
The primary endpoint is to treat the aortic rupture, stop the bleeding and stabilize the hemodynamic status, with the aim to prevent mortality and major cardiac, cerebral, visceral and renal complications. Nevertheless, sub-optimal result may be evident at post-operative examination (CT and MRI): partial apposition of the proximal segment of the endograft (bird beak), evidence of undersized endograft, presence of endoleaks (Figure 6).
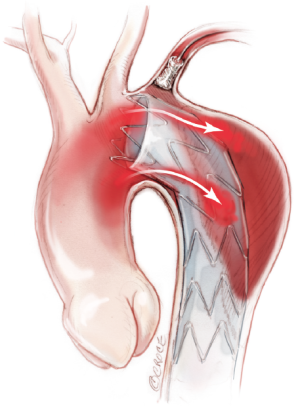
In such cases, a second operative stage need to be planned. This is performed in a patient with a total clinical recover. In order to fix the proximal endograft in a safe and durable way, open aortic arch repair is managed. The distal arch anastomosis is sutured with the proximal tip of the stent graft.
In patients with type B aortic dissection who were already managed with TEVAR, endovascular approach includes the necessity to extend the proximal landing zone into the ascending/arch, using hybrid techniques. However, patients who suffered aortic dissection may have a fragile arch and TEVAR represents only an alternative to surgical management.
Second stage-ascending aorta and total arch replacement (frozen elephant-trunk technique)
Clinical presentation
Normotension (MAP 120/60, Hb >12 g/dL), general good condition.
Exposure and cannulation
Standard median sternotomy is done with aortic care. The exposure and mobilization of supra-aortic vessels is performed. The innominate vein is mobilized or ligated and divided. Intravenous heparin is administrated.
The arterial cannulation is approached via ascending aorta or axillary artery. This procedure facilitates the administration of continuous antegrade cerebral perfusion during deep or moderate hypothermia.
Two staged venous cannula is placed via inferior vena cava and right atrium; left heart vent via right superior pulmonary vein. After cardiopulmonary bypass is initiated, systemic cooling is established. Circulatory arrest is performed between 22-26 °C (bladder temperature).
Bilateral cerebral near-infrared spectroscopy sensors (NIRS) are placed to monitor brain oxygenation during the procedure.
Operation
The ascending aorta and transverse aortic arch are opened. Two balloon-tipped cannulas are placed into the left common carotid artery and the innominate artery to provide selective antegrade cerebral perfusion (Figure 7). In case axillary arterial cannulation, right selective cerebral perfusion is obtained clamping the innominate artery. A cold crystalloid cardioplegia is administrated via the coronary ostia.
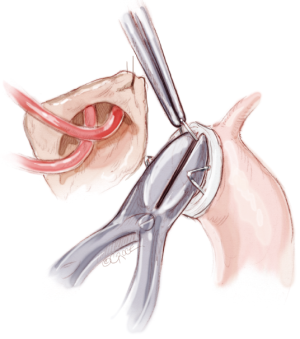
If present, proximal uncovered stents are cut and removed from the endograft (Figure 8).
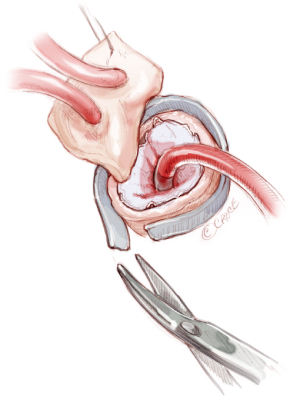
Distal anastomosis is sutured between endograft and Dacron surgical graft and reinforced with outer Teflon strip (Figure 9). Three or four interrupted stiches with pledgets are sutured at polar points to fix the stent-graft before the continuous suture (Figures 10,11). When feasible, the re-implantation of the innominate artery and left carotid artery is managed with an island technique (Figure 12).
Surgical graft is clamped before the origin of the supra-aortic vessels and total cardiopulmonary bypass restarts re-warming the patient. The proximal ascending aorta anastomosis is then sutured.
The ascending aorta is de-aired and unclamped to restore myocardial perfusion.
After adequate re-warming, the cardiac activity is restarted by shock and the CPB is stopped when the temperature reaches 35-36 °C. The CPB cannulas are removed. Atrial and ventricular temporary pacemaker and drainage tubes are placed. Accurate hemostasis and sternal closure are performed at the end of the intervention.
Comments
Ruptured acute type B dissection presenting with hemodynamic instability or shock condition have poor outcome. In this setting, the primary aim is to control the aortic bleeding preventing mortality and major morbidity. The possibility to treat such catastrophic event with endovascular procedures allowed to obtain better in-hospital results compared to open surgery. However planning TEVAR in emergence setting can face with important issues like presence of proximal intimal tear in the left hemiarch and absence of useful and safe proximal aortic neck, undersized aortic diameter at preoperative CT scan related to the hypotension and unavailability of the proper endograft size in that moment.
In some cases, TEVAR represents both the resolution of the acute status and the definitive treatment of the aortic disease.
In other patients, TEVAR can be associated with suboptimal image results, although it is able to stabilize the hemodynamic status, permitting a temporary patient recover. In this situation TEVAR represents the first step of the aortic treatment. The following second stage consists of an open arch repair procedure, that is safer managed in elective status.
In acute and dramatic circumstances, like ruptured type B dissection, TEVAR is a valid and suitable bridge procedure to open surgery, reducing the overall risk for mortality and major complications.
Acknowledgements
Disclosure: The authors declare no conflict of interest.