A systematic review and meta-analysis on pulmonary resections by robotic video-assisted thoracic surgery
Background: Pulmonary resection by robotic video-assisted thoracic surgery (RVATS) has been performed for selected patients in specialized centers over the past decade. Despite encouraging results from case-series reports, there remains a lack of robust clinical evidence for this relatively novel surgical technique. The present systematic review aimed to assess the short- and long-term safety and efficacy of RVATS.
Methods: Nine relevant and updated studies were identified from 12 institutions using five electronic databases. Endpoints included perioperative morbidity and mortality, conversion rate, operative time, length of hospitalization, intraoperative blood loss, duration of chest drainage, recurrence rate and long-term survival. In addition, cost analyses and quality of life assessments were also systematically evaluated. Comparative outcomes were meta-analyzed when data were available.
Results: All institutions used the same master-slave robotic system (da Vinci, Intuitive Surgical, Sunnyvale, California) and most patients underwent lobectomies for early-stage non-small cell lung cancers. Perioperative mortality rates for patients who underwent pulmonary resection by RVATS ranged from 0-3.8%, whilst overall morbidity rates ranged from 10-39%. Two propensity-score analyses compared patients with malignant disease who underwent pulmonary resection by RVATS or thoracotomy, and a meta-analysis was performed to identify a trend towards fewer complications after RVATS. In addition, one cost analysis and one quality of life study reported improved outcomes for RVATS when compared to open thoracotomy.
Conclusions: Results of the present systematic review suggest that RVATS is feasible and can be performed safely for selected patients in specialized centers. Perioperative outcomes including postoperative complications were similar to historical accounts of conventional VATS. A steep learning curve for RVATS was identified in a number of institutional reports, which was most evident in the first 20 cases. Future studies should aim to present data with longer follow-up, clearly defined surgical outcomes, and through an intention-to-treat analysis.
Key words: Robotics; video-assisted thoracic surgery; systematic review; meta-analysis; minimally invasive surgery
Introduction
The ‘minimally invasive’ revolution that began in the 1980s has made a significant impact in many specialties of surgery. The first pulmonary resections by video-assisted thoracic surgery (VATS) were described in the early 1990s (1,2). Since then, there has been growing evidence to suggest that similar or improved long-term oncologic efficacy and survival can be achieved with superior perioperative outcomes by VATS compared to conventional thoracotomy for selected patients with early-stage non-small cell lung cancers (NSCLC) (3,4).
With technological innovation in the form of robotic surgery, robotic video-assisted thoracic surgery (RVATS) emerged as an alternative technique for pulmonary resections in the early 2000s (5,6). Proponents of RVATS emphasize its superior imaging and improved maneuverability compared to conventional VATS, as well as technical advantages such as movement scaling and tremor filtration (7). However, critics of this novel procedure cite its lack of robust clinical evidence as well as its high cost relative to conventional VATS (8). The present systematic review aims to assess the safety and efficacy of pulmonary resections by RVATS, with particular focus on perioperative outcomes, long-term survival and recurrence for malignant lesions. In addition, cost and quality of life (QoL) studies were also systematically evaluated.
Methods
Literature search strategy
Electronic searches were performed using Ovid Medline, EMBASE, Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, and Database of Abstracts of Review of Effectiveness from their date of inception to March 2012. To achieve the maximum sensitivity of the search strategy and identify all studies, we combined “robotics” or “robotic surgery” or “computer-assisted surgery” as Medical Subject Headings (MeSH) terms or keywords with “lung” or “VATS” or “video-assisted thoracic surgery” or “lobectomy” as MeSH terms or keywords. The reference lists of all retrieved articles were reviewed for further identification of potentially relevant studies. All relevant articles identified were assessed with application of predefined selection criteria.
Selection criteria
Eligible studies for the present systematic review included those in which patients with histologically proven NSCLC underwent pulmonary resection by RVATS. For studies that included patients who had NSCLC as a subset of patients who had other pathological entities, results for patients who had NSCLC were extracted if possible. When centers have published duplicate trials with accumulating numbers of patients or increased lengths of follow-up, only the most updated reports were included for qualitative appraisal. It is acknowledged that criteria for patient selection for RVATS varied amongst institutions and sometimes within an institution in different time periods. All publications were limited to human subjects and in English language. Abstracts, case reports, conference presentations, editorials and expert opinions were excluded. Studies that included ten or less patients who underwent pulmonary resections by RVATS were also excluded.
Data extraction and critical appraisal
Findings from initial scoping searches were used to decide outcomes for the present review. The primary outcomes included perioperative mortality and morbidity. Secondary outcomes included quality of life assessment, cost analysis, conversion rate, operating time, intraoperative blood loss, duration of chest drainage, duration of hospitalization, recurrence rate and long-term survival. All data were extracted from article texts, tables, and figures. Two investigators (C.C. and S.A.) independently reviewed each retrieved article. Discrepancies between the two reviewers were resolved by discussion and consensus. The final results were reviewed by the senior investigators (T.D.Y. and C.M.).
Statistical analysis
Meta-analysis was performed by combining the results of reported incidences of any assessed outcomes in comparative studies. The relative risk (RR) was used as a summary statistic. X2 tests were used to study heterogeneity between trials. I2 statistic was used to estimate the percentage of total variation across studies, due to heterogeneity rather than chance. All statistical analysis was conducted with Review Manager Version 5.1.2 (Cochrane Collaboration, Software Update, Oxford, United Kingdom).
Results
Quantity of trials
A total of 393 records were identified through the five electronic database searches. After removal of duplicates and limiting the search to humans and English language, 317 articles remained to be screened. Exclusion of irrelevant studies resulted in 36 articles, which were retrieved for more detailed evaluation. Manual search of references identified three additional potentially relevant studies. After applying the selection criteria, 18 articles remained for assessment (9-26). A summary of these studies from 12 institutions are presented in Table 1. After selecting studies with the most updated data, nine reports were examined in detail, including 941 patients from 12 institutions.
| Table 1 Summary of relevant studies identified in the present systematic review on robotic video-assisted thoracic surgery for pulmonary resections | |||||||
| Institutions | Author | Reference Number | Publication year | Study period | Study type | n | Follow-up (months) |
| MSKCC, NY, USA Milan, Italy Pisa, Italy |
Park* |
(9) |
2012 |
2002–2010 2006–2010 2004–2010 |
ROS |
123 82 120 |
27 |
| Milan, Italy | Veronesi | (10) | 2011 | 2006–2010 | ROS | 91 | 24 |
| Milan, Italy | Veronesi | (11) | 2010 | 2006–2008 | ROS | 54 | NR |
| Pisa, Italy | Melfi | (12) | 2008 | NR | ROS | 107 | NR |
| Pisa, Italy | Melfi | (13) | 2002 | 2001–2001 | ROS | 11 | NR |
| MSKCC, NY, USA | Park | (14) | 2008 | 2007–2007 | ROS | 12 | NR |
| MSKCC, NY, USA | Park | (15) | 2006 | 2002–2004 | ROS | 34 | NR |
| Birmingham, USA | Cerfolio* | (16) | 2011 | 2010–2011 | ROS | 168 | NR |
| Birmingham, USA | Cerfolio | (17) | 2011 | 2009–2010 | ROS | 62 | NR |
| Miami, USA | Dylewski* | (18) | 2011 | 2006–2010 | ROS | 200 | NR |
| Miami, USA | Ninan | (19) | 2010 | 2008–2009 | ROS | 76 | 10.2 |
| Goyang, Korea | Jang* | (20) | 2011 | 2009–2009 | ROS | 40 | NR |
| Innsbruck, Austria | Augustin* | (21) | 2011 | NR | ROS | 26 | 27 |
| Rochester, USA | Fortes* | (22) | 2011 | 2008–2010 | ROS | 23 | 7 |
| Chicago, USA Grosseto, Italy |
Giulianotti* |
(23) |
2010 |
2001–2009 |
ROS |
29 9 |
60 |
| Washington DC, USA | Gharagozloo* | (24) | 2009 | 2004–2008 | ROS | 100 | 32 |
| Washington DC, USA | Gharagozloo | (25) | 2008 | 2004–2007 | ROS | 61 | 28 |
| City of Hope, USA | Anderson* | (26) | 2007 | 2004–2006 | ROS | 21 | 9.8 |
| ROS, Retrospective observational study. NR, not reported. *Updated study included for detailed analysis | |||||||
Surgical Technique and Patient Selection
All nine studies selected for detailed analysis used the same master-slave robotic system (da Vinci, Intuitive Surgical, Sunnyvale, California). The majority of resections were lobectomies, but a smaller proportion of bilobectomies, pneumonectomies, sleeve lobectomies, segmentectomies and wedge resections were also performed. The number of ports used in each institution, as well as the size of the access port/incision used for specimen retrieval, varied between studies. Similarly, the number of lymph node stations dissected and the total number of lymph nodes removed differed between institutions. The majority of patients selected for pulmonary resection had a preoperative histological diagnosis of primary NSCLC with early clinical staging. Other indications for surgery included metastatic disease and carcinoid tumors. A summary of patient baseline characteristics and surgical details are presented in Table 2.
Table 2. After selecting studies with the most updated data, nine reports were examined in detail, including 941 patients from 12 institutions.| Table 2 Summary of surgical details and baseline characteristics of patients who underwent robotic video-assisted thoracic surgery | ||||||||||||||
| Author | Age | Gender (Male) |
Primary NSCLC |
Staging^ | Resection type | Lymph nodes | Access | Port | ||||||
| LR | BR | PR | SR | WR | Stations | Number | ||||||||
| Park | 66 [30-87] | 63% | 325/325 | cI | 324 | 1 |
0 | 0 | 0 | 5 [2-8] | NR | < 8 cm | 3 or 4 | |
| Cerfolio | 67 [21-87] | 45% | 168/168 | NR | 106 | 0 | 0 | 16 | 26 | 8 | 17 | >15 mm | 4 or 5 | |
| Dylewski | 68 [20-92] | 45% | 125/200 | cIA | 106* | 4 | 1 | 35 | 0 | 5 [4-8] | NR | 2-4 cm | 4 | |
| Jang | 64±10 | 58% | 40/40 | cI | 40 | 0 | 0 | 0 | 0 | 7 [2-10] | 22 [7-45] | 2-5 cm | 3 | |
| Augustin | 65 [47-82] | 54% | 24/26 | cI | 26 | 0 | 0 | 0 | 0 | NR | NR | 5-7 cm | 3 | |
| Fortes | 70 [51-86] | 48% | 16/23 | cI-II | 18 | 1 | 0 | 1 | 3 | 4 | 12 [2-50] | 2-3 cm | 3 or 4 | |
| Giulianotti | 66 [16-78] | 50% | 24/38 | cI-II | 32 | 3 | 3 | 0 | 0 | NR | 8 [1-18] | 4-5 cm | 3 or 4 | |
| Gharagozloo | 65±8 | 42% | 100/100 | cI-II | 100 | 0 | 0 | 0 | 0 | 4R; 5L | 12 ± 3 | 2-3 cm | 3 or 4 | |
| Anderson | 67 [36-86] | 52% | 19/21 | cI | 14 | 2 | 0 | 5 | 1 | NR | 16 [2-58] | 3-4 cm | 4 or 5 | |
| *Includes 154 lobectomies, 3 sleeve lobectomies and 3 en bloc resection with lobectomies; ^Majority of patients; NR, Not reported. Resections types: LR, Lobectomy; BR, Bilobectomy; PR, Pneumonectomy; SR, Segmentectomy; WR, Wedge resection; R, Right-sided disease; L, Left-sided disease | ||||||||||||||
Assessment of perioperative outcomes
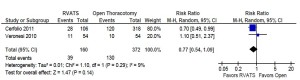
The perioperative mortality rates ranged from 0 to 3.8%. Overall morbidity rates ranged from 10% to 39% and major morbidity rates ranged from 0 to 5% in three studies (9,20,26). The most commonly reported postoperative complications included tachyarrhythmias (3-19%) (9,16,18,21,22,24,26), prolonged air leak (4-13%) (16,18,20-24), pneumonia (1-5%) (18,24) and acute respiratory distress (1-4%) (16,22-24). The conversion rates from RVATS to open thoracotomy ranged from 0 to 19.2%. Average operating time varied between 132 to 238 minutes, whilst blood loss ranged from 30 to 219 mL. The median length of hospitalization was from 2 to 11 days and the duration of chest drainage was 1.5 to 7 days. A summary of perioperative outcomes are presented in Table 3. Jang et al. conducted a three-arm retrospective study comparing 40 patients who underwent RVATS to 40 patients who underwent conventional VATS at the beginning of their institutional experience and 40 patients who underwent conventional VATS after two years of experience, performed by the same surgeon. Their results indicated superior perioperative outcomes for RVATS compared to the first 40 patients who underwent conventional VATS, with fewer complications, shorter hospital stays and lower conversion rates. However, RVATS resulted in similar perioperative outcomes when compared to 40 patients who underwent conventional VATS after 2 years of surgical experience (20). Two retrospective propensity-score analyses comparing RVATS with open thoracotomy for patients with early-stage NSCLC were reported (11,16). A meta-analysis of these two comparative studies assessing perioperative morbidity outcomes identified a trend favoring RVATS compared to conventional thoracotomy (24% vs. 35%, P=0.14), as shown in Figure 1. The length of hospitalization was significantly shorter after RVATS compared to propensity-matched patients who underwent open thoracotomy in both studies. However, RVATS consistently required a significantly longer operative time.
| Table 3 Summary of perioperative outcomes for patients who underwent robotic video-assisted thoracic surgery | |||||||||
| Author | Mortality | Morbidity | Conversion rate |
Operating time (min) |
Blood loss (mL) |
Chest drain (days) |
Length of Total Major Minor stay (days) |
||
| Total | Major | Minor | |||||||
| Park | 0.3% | 25% | 4% | 22% | 8.3% | 206 [110-383] |
NR | 3 [1-23] |
5 [2-28] |
| Cerfolio^ | 0% | 26% | NR | NR | 11.9% | 132±60 | 30±26 | 1.5 [1-6] | 2 [1-7] |
| Dylewski | 1.5% | 26% | NR | NR | 1.5% | 175 [82-370] | 70 [25–500] | 1.5 [1-35] | 3 [1-44] |
| Jang | 0% | 10% | 0% | 10% | 0% | 240±62 | 219±123 | NR | 6 [4-22] |
| Augustin | 3.8% | 15% | NR | NR | 19.2% | 228 [162-375] | NR | 7 [3-15] | 11 [7-53] |
| Fortes | 0% | 39% | NR | NR | 4.3% | 238 [156-323] | 133 [0-2000] | 2 [1-12] | 3 [1-13] |
| Giulianotti | 2.6% | 11% | NR | NR | 15.8% | 209±66 | NR | NR | 10 [3-24] |
| Gharagozloo | 3% | 21% | NR | NR | 1% | 216±27 | NR | NR | 4 [3-42] |
| Anderson | 0% | 29% | 5% | 33% | 0% | 216 [60-384] | 100 [2-600] | 2 [1-5] | 4 [2-10] |
| NR, Not reported; ^62 patients excluded from analysis by author due to conversion (n=13), irresectable disease (n=7) or sublobar resections (n=42) | |||||||||
Assessment of overall survival and recurrence
Survival was calculated from the date of surgery. Of the three studies that presented data on long-term survival for patients with malignant disease, the overall 5-year survival rates ranged from 64% to 80% (9,21,23). An additional study reported an overall survival of 99% after a median follow-up of 32 months (24). Overall recurrence ranged from 0% to 9.8%, including 0% to 4.8% local recurrence, 0% to 6% systemic recurrence, and 0% to 3.8% for both local and systemic recurrence at the time of the latest follow-up. These outcomes are summarized in Table 4.
| Table 4 Summary of long-term survival and recurrence outcomes for patients who underwent robotic video-assisted thoracic surgery for non-small cell lung cancer | |||||
| Author | 5-year survival | Overall recurrence | Local recurrence | Systemic recurrence | Both local and systemic |
| Park | 80% | 9.8% | 2.8% | 5.2% | 1.8% |
| Cerfolio | NR | NR | NR | NR | NR |
| Dylewski | NR | NR | NR | NR | NR |
| Jang | NR | NR | NR | NR | NR |
| Augustin | 63.6% | 7.7% | 3.8% | 0% | 3.8% |
| Fortes | NR | 0% | 0% | 0% | 0% |
| Giulianotti | 71.4% | 4.8% | 0% | 4.8% | NR |
| Gharagozloo | NR | 6% | 0% | 6% | 0% |
| Anderson | NR | NR | 0% | NR | NR |
| NR, Not reported | |||||
Assessment of costs
Park and Flores conducted the only cost analysis to date, comparing conventional VATS (n=87) to RVATS (n=12) to open thoracotomy (n=269) in a retrospective study (14). All direct and indirect expenditures were included to calculate the average hospitalization costs, and the surgeon’s fee was added to calculate the overall cost. This study reported that RVATS was on average $3,981 more expensive than conventional VATS, but $3,988 cheaper than open thoracotomy. After taking into account the amortized cost of employing the robot for each case, an additional $1,715 was required for each patient who underwent RVATS. The increased cost of RVATS compared to conventional VATS occurred almost exclusively on the first day of hospitalization, the reasons for which remained uncertain. Suggested explanations included additional robotic-related equipment and increased likelihood of performing additional procedures, such as bronchoscopy and adhesiolysis. The main factor in reducing the costs of VATS and RVATS compared to thoracotomy was the reduced length of hospitalization.
Assessment of quality of life
Cerfolio et al. reported a quality of life assessment in their propensity-score analysis involving 106 patients with NSCLC who successfully underwent RVATS lobectomy and 318 patients who underwent rib- and nerve-sparing thoracotomy (16). The participants were given the 12-item Short Form Health Survey (SF-12) with supplemental questions about analgesic control at 3 weeks and 4 months postoperatively. Results of this study reported a significantly higher mental QoL score for the RVATS cohort at 3 weeks postoperatively (53.5 vs. 40.3, P<0.001) and a similar trend favoring RVATS for physical QoL score at the same time interval (40.1 vs. 34.1, P=0.07). However, both the mental and physical QoL scores were similar between the two groups at 4 months postoperatively. Pain scores out of 10 was also significantly lower in the RVATS group at 3 weeks (2.5 vs. 4.4, P=0.04). The authors of this study conceded that patients were informed that RVATS was a ‘new and less invasive’ technique, which may have contributed to bias in their reporting.
Discussion
Since the first case-series report on pulmonary resection by RVATS was published in 2002, a number of studies have demonstrated the feasibility of this novel technique with encouraging results (13). Advantages of RVATS compared to conventional VATS include the additional four degrees of freedom (internal pitch, internal yaw, rotation and grip), the elimination of the fulcrum effect, superior 3-D vision from binocular camera, reduced human tremor and improved ergonomic position for the surgeon (12). With these technological improvements, RVATS has the potential to allow more complex procedures such as sleeve lobectomies and chest wall resections to be performed, where conventional VATS might fail (17,27). Indeed, many advocates of RVATS consider it as the leading edge of the swinging pendulum in the paradigm shift towards minimally invasive thoracic surgery (9). On the other hand, critics of RVATS cite the lack of tactile feedback, personnel and cost commitments, as well as prolonged operating time as significant disadvantages of this surgical technique.
The present systematic review identified nine updated retrospective observational studies, mostly from institutions in the United States and Italy involving patients with early-stage NSCLC who underwent lobectomy procedures. These studies reported comparable perioperative outcomes to the results of a recent systematic review on conventional VATS (4). The most common postoperative complications from RVATS, such as tachyarrhythmia, prolonged air leak, pneumonia, and acute respiratory distress, were similar to complications identified for conventional VATS (3). A meta-analysis involving two propensity-score analyses revealed a trend towards fewer complications after RVATS compared to open thoracotomy for selected patients with early-stage NSCLCs. Unfortunately, robust long-term oncologic outcomes such as 5-year survival and disease recurrence rates for patients with malignancies are relatively scarce, with only one small case-series reporting follow-up of more than three years (23). Finally, there is limited but important evidence suggesting superior outcomes in cost and quality of life for selected patients who underwent RVATS compared with propensity-matched patients who underwent open thoracotomy (11,16).
The effect of a steep learning curve for RVATS has been well documented. Perioperative outcomes such as operating time and conversion rates have been shown to significantly improve after the initial learning period. A study by Veronesi estimated the number of operations considered necessary to attain adequate skill in RVATS to be approximately twenty, which is supported by two other institutional experiences (10,13,24). Melfi pointed out that early experiences in RVATS were disadvantaged by a lack of standardized surgical techniques, limited training opportunities, as well as underdevelopment of robotic instrumentation (12). The importance of specialized training for scrub nurses and anesthetists were also highlighted in other studies (12,17). Results from the present systematic review identified the studies with the highest conversion rates (21,23) and operating times (21) were from institutions with fewer than thirty reported cases. This suggests that perioperative outcomes are likely to improve in specialized centers after the initial steep learning curve period. Similarly, these findings may advocate that RVATS should only be performed in tertiary high-volume referral centers with an adequately trained and specialized team of RVATS staff.
A number of limitations exist in the present systematic review. Firstly, it should be acknowledged that publication bias is inherently associated with novel surgical techniques, and unpublished outcomes may differ to the results reported from the selected tertiary centers. Secondly, patient inclusion in each institution was highly selective and variable, and results should be interpreted with caution in view of a lack of randomized-controlled trials comparing RVATS to conventional VATS or open thoracotomy. In addition, many studies presented surgical outcomes without standardized definitions or an intention-to-treat analysis. Examples include the variable definition of ‘conversion rates’, morbidity outcomes, and the exclusion of patients with extensive disease or those who required conversion from statistical analysis. For example, Giulianotti et al. reported one of the highest conversion rates from RVATS to open thoracotomy (6/38, 15.8%) (23). However, three of these conversions were decided after exploratory thoracoscopy and before the robot was docked. In contrast, the multi-institutional report by Park et al. reported a conversion rate of 8.3%, with a definition of ‘conversion’ as the use of open thoracotomy after docking the robot to the patient and initiation of robotic dissection (9). Finally, Cerfolio and colleagues excluded all patients who had conversions (13/168) and those who had metastatic pleural disease (n=7) in their propensity-score analysis comparing RVATS to open thoracotomy (16). Inconsistent reporting of morbidity outcomes was also evident, with only three studies presenting data according to standardized morbidity definitions (9,16,20).
Overall, the current literature suggests that minimally invasive pulmonary resections by RVATS is feasible and can be performed safely for selected patients in specialized centers. However, important questions remain to be answered. Long-term oncologic efficacy compared to open thoracotomy for patients with NSCLC remains to be seen, and the perioperative superiority of RVATS compared to conventional VATS, which is now performed in many centers at a significantly lower cost, is thus far unconvincing. Until such evidence is presented in the form of well-designed randomized controlled trials or a large multi-institutional registry, the role for RVATS will continue to be questioned. Nonetheless, proponents of RVATS highlight the indirect benefits of robotic technology in encouraging the thoracic community to accept and adopt minimally invasive surgery in general (17). Future studies should aim to present long-term follow-up data and use clearly defined surgical outcomes in the form of an intention-to-treat analysis.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Walker WS, Carnochan FM, Pugh GC. Thoracoscopic pulmonary lobectomy. Early operative experience and preliminary clinical results. J Thorac Cardiovasc Surg 1993;106:1111-7.
- Kirby TJ, Rice TW. Thoracoscopic lobectomy. Ann Thorac Surg 1993;56:784-6.
- Cao CQ, Stine ML, Yan TD. True video-assisted thoracic surgery for early-stage non-small cell lung cancer. J Thorac Dis 2009;1:34-8.
- Yan TD, Black D, Bannon PG, et al. Systematic review and meta-analysis of randomized and nonrandomized trials on safety and efficacy of video-assisted thoracic surgery lobectomy for early-stage non-small-cell lung cancer. J Clin Oncol 2009;27:2553-62.
- Ashton RC Jr, Connery CP, Swistel DG, et al. Robot-assisted lobectomy. J Thorac Cardiovasc Surg 2003;126:292-3.
- Morgan JA, Ginsburg ME, Sonett JR, et al. Advanced thoracoscopic procedures are facilitated by computer-aided robotic technology. Eur J Cardiothorac Surg 2003;23:883-7;discussion 887.
- LaPietra A, Grossi EA, Derivaux CC, et al. Robotic-assisted instruments enhance minimally invasive mitral valve surgery. Ann Thorac Surg 2000;70:835-8.
- Swanson SJ. Robotic pulmonary lobectomy--the future and probably should remain so. J Thorac Cardiovasc Surg 2010;140:954.
- Tshomba Y, Melissano G, Civilini E, et al. Fate of the visceral aortic patch after thoracoabdominal aortic repair. Eur J Vasc Endovasc Surg 2005;29:383-9.
- Veronesi G, Agoglia BG, Melfi F, et al. Experience With Robotic Lobectomy for Lung Cancer. Innovations (Phila) 2011;6:355-60.
- Veronesi G, Galetta D, Maisonneuve P, et al. Four-arm robotic lobectomy for the treatment of early-stage lung cancer. J Thorac Cardiovasc Surg 2010;140:19-25.
- Melfi FM, Mussi A. Robotically assisted lobectomy: learning curve and complications. Thorac Surg Clin 2008;18:289-95,vi-vii.
- Melfi FM, Menconi GF, Mariani AM, et al. Early experience with robotic technology for thoracoscopic surgery. Eur J Cardiothorac Surg 2002;21:864-8.
- Park BJ, Flores RM. Cost comparison of robotic, video-assisted thoracic surgery and thoracotomy approaches to pulmonary lobectomy. Thorac Surg Clin 2008;18:297-300,vii.
- Carter RF, McArdle B, Morritt GM. Autologous transfusion of mediastinal drainage blood. A report of its use following open heart surgery. Anaesthesia 1981;36:54-9.
- Cerfolio RJ, Bryant AS, Skylizard L, et al. Initial consecutive experience of completely portal robotic pulmonary resection with 4 arms. J Thorac Cardiovasc Surg 2011;142:740-6.
- Cerfolio RJ, Bryant AS, Minnich DJ. Starting a robotic program in general thoracic surgery: why, how, and lessons learned. Ann Thorac Surg 2011;91:1729-36;discussion 1736-7.
- Dylewski MR, Ohaeto AC, Pereira JF. Pulmonary resection using a total endoscopic robotic video-assisted approach. Semin Thorac Cardiovasc Surg 2011;23:36-42.
- Ninan M, Dylewski MR. Total port-access robot-assisted pulmonary lobectomy without utility thoracotomy. Eur J Cardiothorac Surg 2010;38:231-2.
- Jang HJ, Lee HS, Park SY, et al. Comparison of the early robot-assisted lobectomy experience to video-assisted thoracic surgery lobectomy for lung cancer: a single-institution case series matching study. Innovations (Phila) 2011;6:305-10.
- Augustin F, Bodner J, Wykypiel H, et al. Initial experience with robotic lung lobectomy: report of two different approaches. Surg Endosc 2011;25:108-13.
- Fortes DL, Tomaszek SC, Wigle DA. Early experience with robotic-assisted lung resection. Innovations (Phila) 2011;6:237-42.
- Giulianotti PC, Buchs NC, Caravaglios G, et al. Robot-assisted lung resection: outcomes and technical details. Interact Cardiovasc Thorac Surg 2010;11:388-92.
- Gharagozloo F, Margolis M, Tempesta B, et al. Robot-assisted lobectomy for early-stage lung cancer: report of 100 consecutive cases. Ann Thorac Surg 2009;88:380-4.
- Gharagozloo F, Margolis M, Tempesta B. Robot-assisted thoracoscopic lobectomy for early-stage lung cancer. Ann Thorac Surg 2008;85:1880-5;discussion 1885-6.
- Anderson CA, Hellan M, Falebella A, et al. Robotic-assisted lung resection for malignant disease. Innovations (Phila) 2007;2:254-8.
- Schmid T, Augustin F, Kainz G, et al. Hybrid video-assisted thoracic surgery-robotic minimally invasive right upper lobe sleeve lobectomy. Ann Thorac Surg 2011;91:1961-5.





