Robotic versus conventional sternotomy mitral valve surgery: a systematic review and meta-analysis
Abstract
Background: Robotic-assisted mitral valve surgery (RMVS) is becoming an increasingly performed procedure in cardiac surgery, however, its true safety and efficacy compared to the gold standard conventional sternotomy approach [conventional sternotomy mitral valve surgery (CSMVS)] remains debated. The aim of this meta-analysis was to provide a comprehensive analysis of all available literature comparing RMVS to CSMVS.
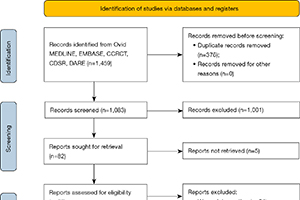
Methods: An electronic search of five databases was performed to identify all relevant studies comparing RMVS to CSMVS. Pre-defined primary outcomes of interest included all-cause mortality, cerebrovascular accidents (CVA) and re-operation for bleeding. Secondary outcomes of interest included cross clamp time, cardiopulmonary bypass (CPB) time, intensive care unit (ICU) and hospital length of stay (LOS), post-operative atrial fibrillation (POAF) and red blood cell (RBC) transfusion.
Results: The search strategy identified fourteen studies qualifying for inclusion in this meta-analysis comparing RMVS to CSMVS. The outcomes of 6,341 patients (2,804 RMVS and 3,537 CSMVS) were included. RMVS had significantly lower mortality when compared to CSMVS group in both the unmatched [odds ratio (OR) 0.33; 95% confidence interval (CI): 0.19–0.57; P<0.001] and matched cohorts (OR 0.35; 95% CI: 0.15–0.80; P=0.01). There was no significant difference in rates of CVA or re-operation for bleeding between the two groups in either the entire included cohort or matched patients. CSMVS had significantly shorter cross clamp time by 28 minutes (95% CI: 19.30–37.32; P<0.001) and CPB time by 49 minutes (95% CI: 36.16–61.01; P<0.001) which remained significantly shorter in the matched cohorts. RMVS had shorter ICU [mean difference (MD) 26 hours; 95% CI: −34.31 to −18.52; P<0.001] and hospital LOS (MD 2 days; 95% CI: −2.66 to −1.37; P<0.001), which were again both significantly shorter in the matched cohort. RMVS group also had fewer RBC transfusions (OR 0.44; 95% CI: 0.28–0.70; P<0.001).
Conclusions: Current evidence on comparative outcomes of RMVS and CSMVS is limited with only low-quality studies currently available. This present meta-analysis suggests that RMVS may have lower mortality and shorter ICU and hospital LOS, however CSMVS may be associated with significantly shorter cross clamp and CPB times. Further analysis of high-quality studies with randomized data is required to verify these results.
Cover