Robotic and endoscopic mitral valve repair for degenerative disease
Abstract
Background: Minimally invasive mitral valve repair has been proven to be a safe alternative to open sternotomy and may be accomplished through classic endoscopic and robotic endoscopic approaches. Outcomes across different minimally invasive techniques have been insufficiently described. We compare early and late clinical outcomes across matched patients undergoing robotic endoscopic and classic endoscopic repair.
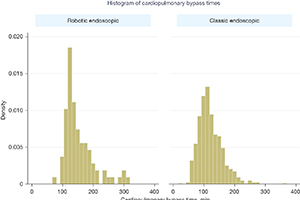
Methods: From 2011 to 2020, 786 patients underwent minimally invasive mitral surgery, from which we were able to generate 124 matched patients (62 patients in each cohort). Clinical results were then compared between the two matched populations. Survival analysis was used to compare freedom from mortality to 10 years among matched classic endoscopic and robotic endoscopic mitral valve repair cohorts and to calculate freedom from moderate or severe mitral insufficiency at latest follow-up. Histograms of cardiopulmonary bypass (CPB) and aortic cross-clamp times were constructed, and mean bypass and cross-clamp times were compared between classic endoscopic and robotic endoscopic cohorts.
Results: There was no difference in early or late mortality at 10 years in either cohort. Freedom from moderate or severe mitral regurgitation or mitral valve replacement at last echocardiogram was 86.4% vs. 73.5% at 10 years, P=0.97. Patients undergoing robotic endoscopic mitral repair had a significantly longer CPB run when compared to the classic endoscopic cohort, with 148 min of CPB in the robotic endoscopic cohort compared to 133 min in the classic endoscopic group, P=0.03. Overall post-operative length of stay was not statistically significant between the robotic endoscopic and classic endoscopic groups, 6.3±0.5 and 6.0±0.3 days, respectively. No patients in either cohort developed renal failure or wound infection. The classic endoscopic group had a slightly higher risk of prolonged ventilation when compared to the robotic endoscopic group, with three classic endoscopic patients remaining intubated >8 hours post-operatively, compared to a single patient in the robotic endoscopic group. There were no unplanned reoperations in either group. Rates of postoperative stroke were comparable between groups (three in the classic endoscopic cohort, and two in the robotic endoscopic cohort).
Conclusions: Index mitral valve surgery via a classic endoscopic approach yields similar clinical outcomes when compared to robotic endoscopic surgery. We demonstrate that both classic endoscopic and robotic endoscopic approaches allow repair of degenerative mitral valves with excellent short- and medium-term outcomes in a tertiary referral center.
Cover