Segmentectomy versus lobectomy for clinical stage IA lung adenocarcinoma
Abstract
Background: Despite the increasingly prevalent early discovery of small-sized non-small cell lung cancers (NSCLCs), particularly adenocarcinoma, sublobar resection has not yet gained acceptance for patients who can tolerate lobectomy.
Methods: We compared the outcomes of segmentectomy (n=155) and lobectomy (n=479) in 634 consecutive patients with clinical stage IA lung adenocarcinoma and in propensity score-matched pairs. Those who had undergone wedge resection were excluded.
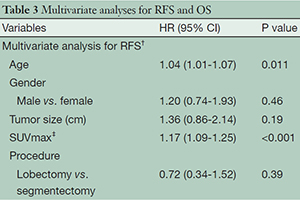
Results: The 30-day postoperative mortality rate in this population was zero. Patients with large or rightsided tumors, high maximum standardized uptake value (SUVmax), pathologically invasive tumors (with lymphatic, vascular, or pleural invasion), and lymph node metastasis underwent lobectomy significantly more often. Three-year recurrence-free survival (RFS) was significantly higher after segmentectomy compared to lobectomy (92.7% vs. 86.9%, P=0.0394), whereas three-year overall survival (OS) did not significantly differ (95.7% vs. 94.1%, P=0.162). Multivariate analyses of RFS and OS revealed age and SUVmax as significant independent prognostic factors, whereas gender, tumor size and procedure (segmentectomy vs. lobectomy) were not. In 100 propensity score-matched pairs with variables adjusted for age, gender, tumor size, SUVmax, tumor location, the three-year RFS (90.2% vs. 91.5%) and OS (94.8% vs. 93.3%) after segmentectomy and lobectomy respectively were comparable.
Conclusions: Segmentectomy with reference to SUVmax should be considered as an alternative for clinical stage IA adenocarcinoma, even for low-risk patients.
Cover