Development of tricuspid regurgitation and right ventricular performance after implantation of centrifugal left ventricular assist devices
Abstract
Background: Tricuspid regurgitation (TR) after left ventricular assist device (LVAD) implantation is associated with a poor prognosis. This study evaluates the development of TR and right ventricular (RV) performance after LVAD implantation.
Methods: Retrospective analysis of patients who underwent LVAD implantation between March 2018 and June 2019. Patients who underwent concomitant tricuspid valve surgery and patients with congenital heart disease were excluded.
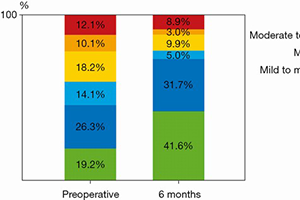
Results: A total of 155 patients underwent LVAD implantation. Fourteen patients were excluded. Of the remaining patients, thirty-one died during the first six months, six were lost to follow-up and two underwent transplantation. 102 patients presented at 6.3 months (5.8 to 7.0). Patients were supported with HeartWare HVAD (74%) or HeartMate 3 (26%). 50.4% were rated as INTERMACS profile 1 or 2. At six months, systolic pulmonary artery pressure dropped from 36 to 21 mmHg (P<0.001). Tricuspid annular plane systolic excursion decreased from 17.3 to 14.3 mm (P<0.001), RV fractional area change did not change (P=0.839). Twenty-two patients (22%) presented with moderate-to-severe or severe (ms-s) TR pre-operatively. Of these, eighteen (81%) showed improvement to ≤ moderate TR. At follow-up twelve patients presented with ms-s TR. Of these, only four patients (33%) had been diagnosed with ms-s TR pre-operatively. There were no differences in pre-operative echocardiographic or clinical parameters between the twelve patients with ms-s late TR and the other ninety patients in the cohort.
Conclusions: TR can show an impressive improvement with LVAD support. Longitudinal RV function decreases; this appears to be compensated by transverse shortening. Late TR can develop independently from pre-operative parameters including TR.
Cover